It’s a familiar story. A class of prescription drugs are being prescribed at skyrocketing ranks. Patients feel like the drugs are harmless and drug makers are assuring doctors of their safety.
This story was the prequel to the opioid epidemic.
And now some medical professionals are advising this may be the intro to the next wave of America’s prescription drug epidemic: medications for anxiety and insomnia.
The Rise of Anti-Anxiety Meds
Over 21% of American Adults (42.5 million) suffer from anxiety disorders. Many of them are using benzodiazepines to treat these disorders. You may know these medications as Xanax, Klonopin, Valium, and Ativan.
Anxiety disorders are the most common and pervasive mental health disorders in the United States, according to the Anxiety and Depression Society of America (AADA). So it comes as no surprise that benzodiazepines are one of the most widely prescribed medications in the U.S., particularly among certain age groups.
Between 1996 and 2013, the number of adults filling a benzodiazepine prescription increased by 67%.
According to a study published by the National Library of Medicine, 30.6 million adults (12.6%) reported past-year benzodiazepine use annually, roughly 1 in 10 adults. Of that group, 5.3 million adults (2.2%) reported misuse, a little under 1 in 5 users.
Benzodiazepines, or benzos, work by triggering a tranquilizing chemical in the brain. When someone feels anxious, the brain can get excited and overactive. Anti-anxiety medications enhance a tranquilizing neurotransmitter, GABA, that slows down brain activity and reduces symptoms of anxiety. Medications like benzodiazepines add to the calming effect and keep the brain calm. Benzodiazepines are also commonly used as a short-term treatment for insomnia.
The Side Effects and Dangers of Anti-Anxiety Medications
Anti-anxiety medications are used to treat a range of neurological and psychological disorders, including anxiety disorders, panic attacks, and insomnia. But they’re not without risk.
Side Effects
Side effects of anti-anxiety medications can include
- Drowsiness
- Confusion
- Dizziness
- Trembling
- Vision problems
- Impaired coordination
- Grogginess
- Headaches
- Depression
Among older individuals, medical benzodiazepine use poses risks of serious adverse effects, including impaired cognitive functioning, reduced mobility and driving skills, and increased risks of falls.
Dependency
Benzos are typically meant for short-term use only. Just like opioids, chronic use of benzodiazepines can lead to tolerance and severe withdrawal symptoms that can last for months after the medication has been discontinued.
Benzodiazepine withdrawals can include sleep disturbance, irritability, increased tension and anxiety, panic attacks, hand tremor, sweating, difficulty in concentration, dry retching and nausea, some weight loss, palpitations, headache, muscular pain and stiffness, and a host of perceptual changes.
Withdrawal can also bring more serious developments, such as life-threatening seizures and psychotic reactions.
Several studies have shown that a substantial portion of benzodiazepine use is long-term, despite increased awareness of and caution regarding the risks of long-term use.
Overdose
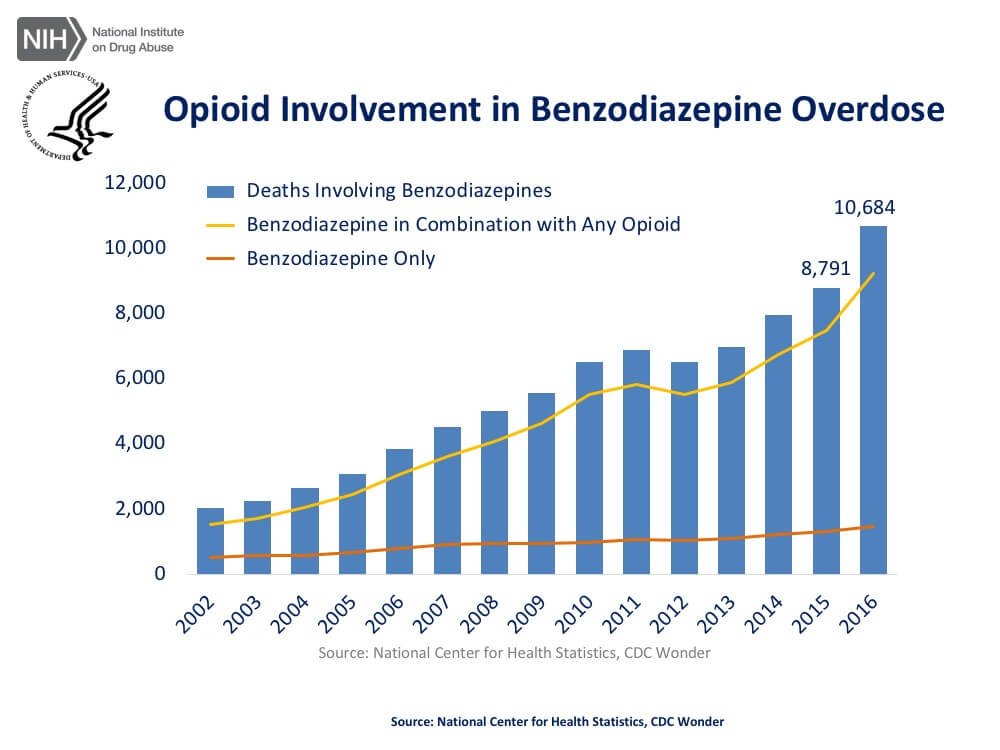
The number of prescriptions for anti-anxiety medications isn’t the only thing on the rise: the rate of overdose deaths involving benzodiazepines rose from 1,135 cases in 1999 to 12,499 cases in 2021, an increase of over 1,000%.
One of the biggest factors in the rise of benzodiazepine overdose deaths is the combined use of opioids and benzodiazepine.
Research by the National Institute of Drug Abuse reports that 16% of overdose deaths due to opioids also involved benzodiazepines. The overdose death rate among patients taking both types of medication was 10x higher than among those only taking opioids.
“The risk of overdose and death from benzodiazepines themselves is generally low-to-moderate in otherwise healthy adults,” Dr. Gary Reisfield, professor of psychiatry at the University of Florida told CNN. In combination with other sedatives such as opioids or alcohol, “their lethality is magnified,” Reisfield said.
Suicide
In May 2017, musician Chris Cornell committed suicide in a hotel room in a Detroit hotel room. After the cause of death was announced, his wife made a public statement blaming the Soundgarden lead singer’s anti-anxiety medication for his suicide.
Though rare, researchers have found an increased risk of suicide associated with the use of anti-anxiety medications.
Benzodiazepines have been shown to increase aggression and impair behavioral inhibitions, according to a review titled Prescribed Benzodiazepines and Suicide Risk. In particular, benzodiazepines may promote a disassociated type of aggression where users perceive themselves as friendlier and less hostile but then respond in a more aggressive way to provocation. Both impulsivity and aggression have been linked to suicide risk.
Benzodiazepine withdrawal symptoms may also contribute to suicide risk, suggest the study authors, since stopping the medication can increase anxiety and insomnia.
In some cases, benzodiazepines can be the instrument for suicide. As mentioned before, high doses can lead to lethal respiratory suppression, particularly when combined with opioids or alcohol.
Populations at Highest Risk from Anti-Anxiety Medication Dangers
As the rates of anti-anxiety medication prescriptions and overdose deaths both rise, some populations are more at risk than others, particularly women, the elderly, and teens.
Women are Twice as Likely to be Prescribed Anxiety Meds
Women are among the hardest hit by the opioid epidemic, and it seems that the benzo epidemic is following suit.
Women tend to use anti-anxiety medications at a higher rate than men.
According to the America’s State of Mind report, women have the highest utilization rate of anti-anxiety medications. This problem also sees disparities in prescribing rates as well. In 2020, a study found that male prescribers were more likely to prescribe benzodiazepines to female patients relative to male patients.
Older Adults Prescribed Anti-Anxiety Meds More than Any Age Group
For most older adults, the risks of benzodiazepines far outweigh the benefits and can even be life-threatening, researchers say. Yet data shows that patients over 65 receive more prescriptions for these anti-anxiety drugs than any other age group. And one-third of older adults who receive benzodiazepines are using them long-term (more than 120 days a year).
Female patients over 65 are prescribed benzodiazepines at nearly twice the rate as male patients in the same age group.
Benzodiazepine use is associated with a significantly increased risk of falls and fractures. Older adults with osteoporosis, sensory loss (eg, decreased vision, peripheral neuropathies), muscle weakness, Parkinson’s disease, arthritis, polypharmacy, and orthostasis, patients who frequently use the restroom at night, and those with a history of falls are particularly vulnerable to falls and fractures when taking benzodiazepines, according to the Mayo Clinic.
Benzodiazepines may even lead to dementia and cognitive decline in older adults. These medications can cause short-term cognitive deficits, particularly in memory, learning, attention, and visuospatial ability, and they are also associated with the development of lasting cognitive deficits and dementia.
Several studies have indicated that even after benzodiazepines are discontinued, the cognitive function of long-term users continues to be impaired, suggesting lasting and possibly irreversible cognitive deficits from benzodiazepine use.
The safety risks for benzodiazepine use in the elderly are so great that the American Geriatrics Society placed them on the list of medications that should be avoided by people 65 and older, and several major psychiatric associations advise against using them for general anxiety disorder or insomnia in the elderly.
Teen Use of Anti-Anxiety Medications Can Lead to Rx Misuse
Teens prescribed anti-anxiety or sleep medications may be up to 12 times more likely to abuse those drugs illegally than teens who have never received a prescription, according to research by the American Psychological Association (APA).
“The public often thinks that nonmedical use of these prescription drugs is driven by doctor shopping and drug dealers, but it isn’t,” said lead researcher Carol J. Boyd, Ph.D., a professor at the University of Michigan School of Nursing.
“It is driven by people with prescriptions who divert their pills to other people, who are usually friends or family members."
The prescribing of anti-anxiety and sleep medications to teens has increased over the past decade, along with the abuse of these drugs, according to several studies. A study published in the journal Pediatrics found a significant increase in children and teens diagnosed with anxiety during office visits, but a decrease in the proportion receiving therapy, which included counseling or psychotherapy.
Despite the nearly 4x increase in anxiety disorder in children, the study found the proportion of therapy visits decreased from 48.8% to 32.6%, while the proportion of children prescribed anxiety medications remained the same.
Preventing the Next Prescription Epidemic
Is there still time to prevent benzodiazepines from becoming the next prescription drug epidemic, or is it already too late?
Lessons learned from the opioid epidemic can be applied to the shadow epidemic of anti-anxiety medication. For example, a greater awareness of the potential side effects, such as tolerance and dependence, on the part of prescribers can go a long way.
According to researchers, the majority (55%) of benzodiazepine prescriptions come from primary care physicians, while only (16%) come from psychiatrists. A limited number of studies have shown that cognitive behavior therapy (CBT) can be just as effective as a pharmacological treatment for generalized anxiety disorder and can be better tolerated by patients.
Cognitive behavior therapy can also be an effective treatment for insomnia. Recent guidelines from the American College of Physicians recommend cognitive behavior therapy before medication to treat insomnia.
If more primary care physicians began prescribing CBT for anxiety or insomnia rather than immediately writing prescriptions for benzodiazepines, it could reduce the amount of Americans turning to a potentially addictive drug.
Anti-anxiety medications can be helpful in the treatment of anxiety disorders and insomnia, but these powerful medications come at a risk.
Safe Use of Benzodiazepines
If you’re considering asking for a benzodiazepine prescription, or your doctor has already written one for you, these guidelines can help protect you and the members of your household:
- Be aware: know the side effects and risks of benzodiazepine use
- Use as directed: don’t increase your dosage or continue longer than recommended by your doctor
- Don’t stop cold turkey: if you’re ready to stop benzo use, taper your usage under the supervision of your doctor.
- Don’t mix meds: benzodiazepines can be extremely dangerous when mixed with opioids, alcohol, and other central nervous system depressants
- Lock your meds: if you have a benzo prescription, lock it up securely to keep it safe from experimental teens or curious toddlers
- Don’t share: benzodiazepines have a large risk for dependency and withdrawal, so don’t share your Rx with anyone.
- Seniors: use with caution: if you’re over the age of 65, talk to your doctors about the increased risks of senior benzodiazepine use.
The next prescription drug epidemic is sneaking up on America, one anti-anxiety prescription at a time. It’s time to spread awareness of the potential risks that can come from benzodiazepine medications and to take steps to protect ourselves and our loved ones if we’ve chosen to use these powerful and potent medications.
This blog post was updated for 2023 to reflect current data, statistics, and prescribing information.